Point-of-care testing (POCT) is a tool that can improve patient satisfaction, understanding, and engagement. Our healthcare environment advances when we encourage patients to make decisions that improve their health and population health programs benefit from initiatives that improve patient engagement.
Learn how laboratory professional oversight of POCT can enhance POCT’s ability to positively impact patient engagement and outcomes.

As healthcare continues to evolve to a more patient-centric, proactive practice of medicine, laboratories must evaluate how they fit into the overall value proposition. Many healthcare organizations (HCOs) are adopting population health management (PHM) strategies to adapt to value-based care and improve the overall health status of their patient population. An integral part of PHM is engaging patients as active members of their own care team and finding ways to encourage them to make good health decisions.
One tool that can drive patient engagement in certain patient scenarios is point-of-care testing (POCT), and it can have a positive impact on both health outcomes and spending. POCT is growing in popularity and in response to the overall changes in healthcare. As HCOs attempt to encourage patients to make decisions that improve their health and help them have a greater understanding of their chronic diseases, POCT comes into the picture as a tool that improves patient understanding and engagement. See Figure 1.
The Shift to Proactive & Preventive Healthcare

Myriad problems within our healthcare system have the potential to be improved upon with advanced technology and rapid growth of digital and virtual health tools. The need to shift from an expensive, reactive healthcare environment to one that is proactive and focused on creating an environment more conducive to preventive care and healthy choices creates an opening for new technologies to engage patients. These trends—new technologies and patient-centered care—are leading us away from a centralized system to a more flexible system that includes care interventions at the patient’s location,
which means care that is more accessible and affordable. This shift to a value-based system where payments are centered on keeping populations healthy and out of the hospital mandates that care interventions take place where it is best for the patient. This new system includes comprehensive PHM supported by tools and interventions that drive patient engagement, such as POCT, remote patient monitoring, mobile health apps, and televisits.
Population Health Management
Patient engagement, quality scorecards, and PHM are the “foundational pillars” that can help improve quality of care.1 In an effort to improve quality of care, HCOs are developing PHM programs that identify and address care gaps in an increasingly effective way. Currently, these programs move toward value-based care, yet still allow for revenue from traditional fee-for-service (FFS) contracts. Many PHM initiatives involve laboratory data and POCT results. Figure 2 outlines the basic steps involved in developing a PHM program.
Patient Engagement—Crucial for PHM
A big factor in implementing a population health program is creating and maintaining proactive patient engagement. It is well recognized that engaged patients have better health outcomes and spend fewer healthcare dollars. Because of this understanding, the need for greater patient engagement is a prevailing theme among today’s HCOs. Patient engagement strategies can improve patient experience by helping patients become more active participants in their care. Ideally, providers interacting with engaged patients can use shared decision-making to review available interventions and build patient preferences into treatment decisions.
User-Centric, Personalized Patient Engagement Works Best
 Engaging patients is not an easy task; there is no one-size-fits-all engagement method or magic app. Partners HealthCare in Boston has been on the leading edge of using telemedicine and mobile apps to motivate patients. Through trial and error, Partners learned that patient engagement is complex. With behavioral psychology and user-centered design principles, Partners developed a program that helps patients with type 2 diabetes become more active. Activity levels, location, weather, and patient interest level are tracked alongside blood glucose levels to offer personal messages that are intended to motivate patient activity. Partners is already seeing improvements in its diabetes patients.2
Engaging patients is not an easy task; there is no one-size-fits-all engagement method or magic app. Partners HealthCare in Boston has been on the leading edge of using telemedicine and mobile apps to motivate patients. Through trial and error, Partners learned that patient engagement is complex. With behavioral psychology and user-centered design principles, Partners developed a program that helps patients with type 2 diabetes become more active. Activity levels, location, weather, and patient interest level are tracked alongside blood glucose levels to offer personal messages that are intended to motivate patient activity. Partners is already seeing improvements in its diabetes patients.2
In another patient engagement success story, Atrium Health in North Carolina and South Carolina is using remote patient monitoring combined with a health coach to help patients develop personal health goals. These goals are then added to Twine, its health platform app, which sends patients reminders and tracks progress toward goals. Early results show promising results for Atrium’s hypertension patients.2
Yet many patients and providers still fall into the old patterns of a paternalistic system. It takes focused effort to raise patient interest levels and engagement and to encourage patients to take a greater responsibility for their healthcare.3
POCT & Patient Engagement
It is widely accepted that patients who are actively engaged in their healthcare have improved health outcomes, and POCT is a tool known to improve patient engagement. Any intervention aimed at increasing a patient’s understanding and motivation level influences patient engagement.3 In general, patients have a positive perception of POCT because of its mobility and convenience. The ready availability of POCT results helps patients better understand their conditions and can lead to insights about how certain actions affect their health. While the laboratory may not be considered directly linked to patient engagement, laboratory oversight of POCT can play a role.
POCT’s Renewed Value
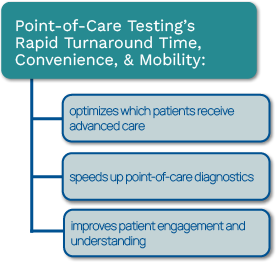
Major growth in POCT is expected as technologies improve and POCT benefits are realized in the new healthcare paradigm. The benefits that POCT offers have a renewed importance in patient-centered, value-based care. The rapid turnaround time (TAT), convenience, and mobility that POCT offers:
- optimizes which patients receive advanced care
- speeds up point-of-care diagnostics
- improves patient understanding and engagement; see Figure 3.
POCT’s Potential to Influence Outcomes & Downstream Costs
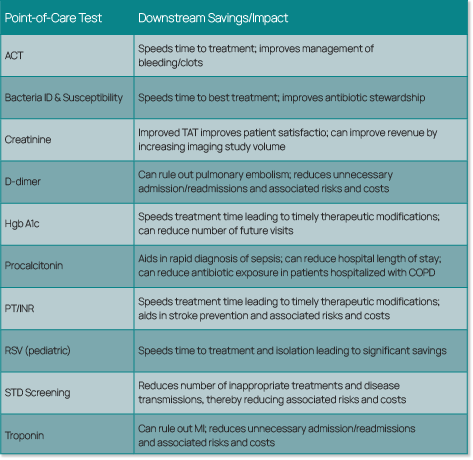
It becomes important to grade the value of the tests by their influence on patient outcomes rather than only on costs. It is no surprise that POCT, without the economy of scale created by volume and automation that occurs in larger centralized lab testing, is more expensive when comparing direct costs. Yet POCT can have a positive influence on patient-centered care and increase the level of patient engagement. In addition, properly placed POCT offers opportunities for significant downstream savings in avoided procedures, risks, and complications. Looking at downstream savings, there is a great potential for POCT to have a significant impact on healthcare costs with something as simple as eliminating a clinic visit.4 In most HCOs, much of what is performed at the point of care is still done on an FFS basis. As we continue to move toward value-based care and contracts in addition to POC revenue, we have to look at overall patient outcomes to see the full value of POCT.
Rapid TAT Can Help Speed Treatment & Avoid Unnecessary Risk
Studies have shown that reducing the TAT for cardiac marker testing from two hours to 10 minutes can decrease hospital length of stay and improve overall Emergency Department (ED) productivity.5 Also, it has been repeatedly demonstrated that POCT can speed time to diagnosis and corresponding treatment (e.g., pregnancy test or creatinine to allow for faster imaging studies). Certain POCT, such as pediatric influenza or a bacterial ID, has been shown to improve the appropriateness of antibiotic use. POCT lactate has been associated with reduction of mortality and ICU admissions for sepsis patients.5 Troponin and D-dimer testing has been helpful in screening for myocardial infarction (MI) and pulmonary embolism to avoid unnecessary admissions/readmissions. See Figure 4 for several examples.
Telemedicine & mHealth on the Rise
 Taking POCT to the next level, patient engagement is also greatly enhanced by telemedicine and mobile health (mHealth) apps. The ability for patients to participate in televisits with their providers and to monitor their symptoms with wireless devices is making it less necessary to visit providers within hospitals or clinics for certain conditions.
Taking POCT to the next level, patient engagement is also greatly enhanced by telemedicine and mobile health (mHealth) apps. The ability for patients to participate in televisits with their providers and to monitor their symptoms with wireless devices is making it less necessary to visit providers within hospitals or clinics for certain conditions.
In one example, Johns Hopkins has a Hospital at Home (HaH) program that leverages remote monitoring tools and in-home caregiver visits to track patient conditions within the comfort of their homes rather than in the hospital.6
In another example, Geisinger Health is practicing community paramedicine through its Mobile Health Team of paramedics and EMTs who use ambulances as mobile health clinics that travel to areas that are convenient for patients.6
In a final example, Bryan Health in Lincoln, Nebraska, implemented a user-friendly, online diagnosis and treatment platform to improve urgent care access for minor health concerns. Patients pay a low-cost fee to connect with a board-certified physician through the mobile Bryan Health ezVisit tool.7
Innovative endeavors such as these extend the reach of providers and improve the patient experience.
Closing Care Gaps
An effective PHM program identifies and uses the appropriate tools and staff to “close care gaps.” Many time-sensitive screening, preventive care, and health maintenance interventions can be considered gaps in care when they are missed. For example, pneumonia and influenza immunizations in the elderly population, as well as screening exams for cancer (e.g., breast, colon, prostate) or chronic disease (e.g., diabetes, hypertension, osteoporosis), are effective preventive care measures. Today’s savvy HCOs are proactively addressing these care gaps using data analytics to define interventions and are continuing to improve their programs as new information is gathered.
HCOs on average spend $40,000 per year per physician, and the staff spends about 15 hours each week working to close care gaps as part of quality measure reporting.1 As risk-based contracts increase, the time spent closing care gaps and addressing quality initiatives is expected to increase.
CPT II Codes to Document Care Gap Closure
One way in which care gap closure is being documented for payers is with the use of CPT Category II codes. CPT II codes are a new version of Current Procedural Terminology (CPT) codes that are used to assess Healthcare Effectiveness Data and Information Set (HEDIS) and Star rating scores. HEDIS is a set of standardized performance measures developed by the National Committee for Quality Assurance (NCQA) that is used to measure and compare quality across health insurance plans. The Centers for Medicare & Medicaid Services (CMS) Five-Star Quality Rating System is used to measure the quality of care for Medicare Advantage (MA) and Prescription Drug Plan (Part D) beneficiaries. Both HEDIS and Star ratings affect HCO reimbursements and they are improved by:
- encouraging patients to have preventive health visits, screenings, and tests
- educating patients about medication adherence and side effects
- reaching out to those who are non-compliant
![]()
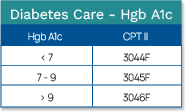
CPT II codes are used to “grade” performance. As “follow-up” codes, CPT II codes provide additional information to the insurance provider that demonstrates the level of quality. For example, in tracking Hgb A1c levels for diabetic patients, the CPT II codes correspond to the Hgb A1c result (see Figure 5), showing the insurance company where the patient stands regarding their diabetes. Laboratory professionals need to be aware of these types of reimbursement policies and determine where lab data applies.
For diabetic patients, the HEDIS program recommends that patients receive screening for diabetic retinopathy because diabetes can affect the blood vessels in the retina. Recently, Gateway Medical Associates in Pennsylvania implemented a telemedicine solution to administer diabetic retinopathy exams (DREs). Gateway partnered with Intelligent Retinal Imaging Systems (IRIS) to develop this telemedicine solution that has enabled Gateway to advance HEDIS compliance, improve patient care, and increase quality incentive revenue. Gateway’s DRE compliance rate has increased from 37% to 85%.8
How These Trends Affect the Laboratory
The way healthcare is delivered is shifting, causing the how and where of laboratory testing to change as well. POCT is anticipated to continue growing in volume and in its ability to impact downstream costs and patient engagement. Imagine the laboratory of the future where POCT has taken the place of certain core lab tests so that the central lab can effectively handle high-volume, high-impact testing for the most critical patient population.
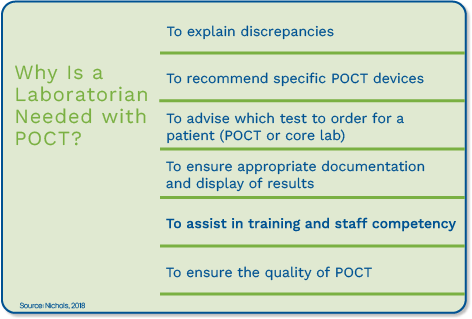
POCT Quality Improves with Laboratory Professional Oversight
Imagine the laboratory professional providing valuable insights about the best POCT devices and the most beneficial POCT patient opportunities, and ensuring an overall top-quality POCT program. As the demand for POCT grows, testing must follow the same path of quality as central laboratory testing. Laboratory professionals are well-equipped with the knowledge base to ensure POCT is applied in the appropriate patient scenarios and that test results meet quality requirements. See Figure 6.9
POCT Access Improves with Integration
In addition to placing the right POCT in the right places, there must be processes in place that ensure the care team members who need to act on the results have real-time access. Because the true value of POCT is realized in its rapid TAT, for those results to be immediately available to caregivers, it is imperative that POCT results are integrated into the EHR. Fast TAT is not effective if the results do not get to the caregiver in time to impact faster care decisions. Interfacing POCT devices to a POCT management software can improve access to results, enabling and enhancing the feature of POCT that makes it desirable rapid TAT. Diagnostic accuracy, quality management, and operational processes that enable fast access to results are crucial components of getting the most out of your POCT.5 The National Institutes of Health acknowledged that POCT’s ability to enable providers to make rapid decisions at the patient’s side has tremendous potential to help improve our healthcare system and the way we deliver care.10
Working Together
 For these improvements to happen, laboratory professionals, patients, and providers must be engaged. This means POCT manufacturers must do their part by designing devices that are interfaceable, intuitive, and easy to use. And laboratory professionals must do their part by being actively involved in decisions about where POCT can have the greatest influence on patient care and about selection and implementation of reliable systems. Laboratory professionals and nurses who are involved in POCT can work together with an aligned vision for the POCT program. Certain actions from the point-of-care coordinator can smooth the teamwork relationship. These actions include explaining the “why” behind POCT activities (e.g., QC and proficiency testing), developing streamlined QA requirements that take into account resources, and writing policies and procedures in a user-friendly (i.e., non-lab lingo) manner.9
For these improvements to happen, laboratory professionals, patients, and providers must be engaged. This means POCT manufacturers must do their part by designing devices that are interfaceable, intuitive, and easy to use. And laboratory professionals must do their part by being actively involved in decisions about where POCT can have the greatest influence on patient care and about selection and implementation of reliable systems. Laboratory professionals and nurses who are involved in POCT can work together with an aligned vision for the POCT program. Certain actions from the point-of-care coordinator can smooth the teamwork relationship. These actions include explaining the “why” behind POCT activities (e.g., QC and proficiency testing), developing streamlined QA requirements that take into account resources, and writing policies and procedures in a user-friendly (i.e., non-lab lingo) manner.9
Summary
For many years, laboratory professionals have been encouraged to step outside of their comfort zones and to integrate their ideas and knowledge throughout their facilities. Today’s changing healthcare landscape reiterates this need and opens new opportunities for laboratories. At a minimum, laboratorians should be aware of the healthcare terrain, be familiar with terms and initiatives, such as population health and patient engagement, and should try to understand where and how the laboratory fits in these value-focused programs.
In the past, many laboratory professionals have avoided POCT oversight because of the complexity and abundance of challenges inherent to POCT, added on top of an already full schedule of duties in the laboratory. However, stepping back and looking at the bigger picture, it is time to reevaluate POCT, thinking of your patient population and specialty, to determine where POCT can support PHM, improve patient engagement, eliminate risks, or reduce downstream spending. Laboratory testing is “changing with the times” and POCT is going to continue to gain acceptance. Do you have an opportunity to step in and make improvements in your facility’s POCT program? Thinking of PHM and patient engagement, are there areas where a POC test could improve patient care in your HCO?
Orchard Software Supports Point-of-Care Testing
At Orchard, we pride ourselves on researching and developing software tools that laboratory professionals can use to make their jobs easier and more productive, and that allow them to showcase their value. We are also in tune with current healthcare and industry trends. These two factors have led to the development of our POCT integration and management software, Orchard® Point-of-Care™.
Orchard Point-of-Care is designed for remote oversight of POCT, supporting centralized governance of a comprehensive POCT program across all patient testing locations. Orchard solves many of the problems associated with POCT management by enabling remote oversight to track patient testing, devices, operator certifications, and QC. Orchard also integrates POCT into the EHR to allow immediate access to results and to automate the billing process. From a value-based quality initiative perspective, Orchard can support the addition of CPT II codes to close care gaps, helping to ensure maximum reimbursement. In an FFS scenario, Orchard automates POCT billing as tests are completed, making sure every POCT is appropriately billed. In today’s healthcare organizations, the complexity of POCT greatly benefits from a comprehensive management and integration software tool that integrates with the EHR, supports billing, and allows remote oversight of all POCT activities. For more information, visit www.orchardsoft.com or call (800) 856-1948.
References
- Finocchiaro, P. (2017, January). Five ways to close gaps in care and build a successful quality improvement program. Managed Healthcare Executive. Retrieved from http://www.managedhealthcareexecutive.com/managed-healthcare-executive/news/five-ways-close-gaps-care-and-build-successful-qualityimprovement-program?page=0,0
- Van Dyke, M. (2018, May). Providers aim to build engagement tools that actually work. Health Data Management. Retrieved from https://www.healthdatamanagement.com/news/providers-aim-to-buildingengagement-tools-that-actually-work
- Carman, K. L., Dardess, P., Maurer, M., Sofaer, S., Adams, K., Bechtel, C., & Sweeney, J. (2013). Patient and family engagement: A framework for understanding the elements and developing interventions and policies. Health Affairs, 32(2), 223-231. http://dx.doi.org/10.1377/hlthaff.2012.1133
- St John, A., & Price, C. P. (2013). Economic evidence and point-of-care testing. The Clinical Biochemist Reviews, 34(2), 61–74. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3799220/
- St John, A., & Price, C. P. (2018). Benefits of point-of-care testing in the Emergency Department. Acute Care Testing. Retrieved from https://acutecaretesting.org/en/articles/benefits-of-point-of-care-testingin-the-emergency-department
- Wiler, J. L., Harish, N. J., & Zane, R. D. (2017). Do hospitals still make sense? The case for decentralization of health care. Catalyst New England Journal of Medicine. Retrieved from https://catalyst.nejm.org/hospitals-case-decentralization-health-care/
- American Hospital Association. (2018, February). Members in action case study: Virtual urgent care | Bryan Health. Retrieved from https://www.aha.org/system/files/2018-02/bryan-health-virtual-urgent-care.pdf
- HMT Mag. (2018, August). Gateway Medical Associates closes care gaps and improves patient outcomes with IRIS diabetic retinal exam telemedicine program. Health Management Technology. Retrieved from https://www.healthmgttech.com/gateway-medical-associates-closes-care-gaps-and-improves-patientoutcomes-with-iris-diabetic-retinal-exam-telemedicine-program
- Nichols, J. (2018, August 21). The nursing-lab relationship in POCT: The good, the bad, and the ugly of interdisciplinary teams. Whitehat Communications Webinar. Retrieved from https://www.whitehatcom.com/POC_Group_Webinars_2018.htm
- Preston, J. (2017, March). Living in the moment: Point-of-care market tops $18B. MedCity News. Retrieved from https://medcitynews.com/2017/03/point-of-care-market-tops-18b/?rf=1

