Abstract
POCT is gaining popularity in scenarios where rapid turnaround time outweighs testing limitations. As POCT programs grow, effective oversight is best achieved by understanding end users’ perspectives and culturing a spirit of teamwork.
The year 2020 has certainly held its share of challenges specific to healthcare, with the coronavirus pandemic top of the list. Point-of-care testing (POCT) continues to gain traction and prove its place as part of an overall effective testing plan to help manage patient care, particularly in light of the COVID-19 pandemic. Laboratory professionals, as stewards of proper laboratory testing, are responsible for the proper use and implementation of POCT. This responsibility is best embraced by affecting a culture of teamwork and understanding POCT from the end user’s perspective.
Executive Summary
- POCT continues to increase in demand, particularly in patient scenarios that benefit from a rapid turnaround time (TAT), such as COVID-19 testing.
- POCT also plays an important role in value-based care, patient satisfaction, patient engagement, and population health management.
- POCT plays an important role in the healthcare system’s shift to bring care closer to the patient and take patient situational circumstances into account when determining treatment plans.
- POCT allows for quick medical decisions, early diagnosis, and subsequent early treatment that leads to improved health outcomes.
- Laboratory professionals, as stewards of proper laboratory testing, are responsible for the proper use and implementation of POCT.
- Laboratory professionals have the best-fit knowledge base to oversee an effective POCT program.
- The responsibility of POCT oversight is best embraced by affecting a culture of teamwork and understanding POCT from end users’ perspectives.
- The increased demand for POCT offers an opportunity for lab professionals to increase their contribution to patient care, bringing visibility and respect to the field.
Healthcare in 2021
 Even prior to the COVID-19 pandemic, the healthcare industry has been slowly, but steadily, shifting away from volume-based care to value-based care with
Even prior to the COVID-19 pandemic, the healthcare industry has been slowly, but steadily, shifting away from volume-based care to value-based care with
a focus on patient outcomes, patient-centered care, patient engagement, patient experience, and population health management. In some ways, the pandemic has accelerated this value-based care movement, particularly in the acceptance of telemedicine and mobile app use.
The COVID-19 crisis has been added to the top of a long list of challenges that healthcare administrators face. Figure 1 lists the top challenges for healthcare leaders in 2020.
Among these healthcare challenges, there is a clear shift to move care processes closer to the patient and take patient situational circumstances into account when determining treatment plans. POCT plays an important role in this move to bring care closer to the patient.

Rapid TAT Makes POCT Valuable
POCT has been steadily gaining in popularity—being accepted and requested more often by providers and patients. Rapid POCT results near the patient facilitate improvements in diagnosis, monitoring, and disease management. POCT allows for quick medical decisions, early diagnosis, and subsequent early treatment that can lead to improved health outcomes.
One reason for POCT’s increasing popularity is that the technology is becoming more sophisticated and less error-prone for end users. There continues to be developments in the technologies that underlay POCT (e.g., biosensors, microfluidics, bioanalytical platforms, assay formats, lab-on-a-chip technologies, etc.). For example, there are advancements in POCT technologies related to genetic testing, such as POC tests to detect Clostridium difficile or to uncover a CYP2C19 mutation that reduces effectiveness of an antiplatelet aggregation medication.2
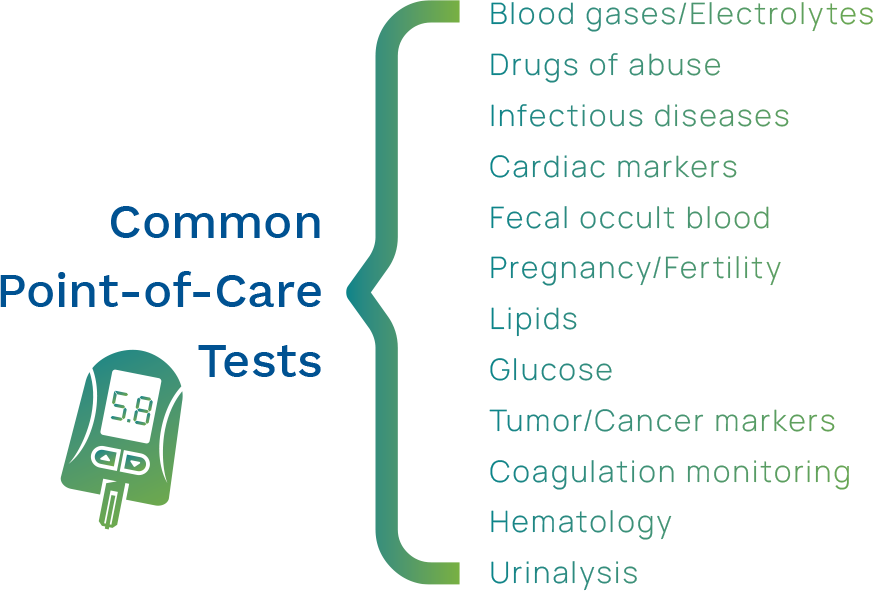
Currently, POC tests are available for any number of common healthcare scenarios (see Figure 2), as well as a number of less mainstream testing, such as:
- Biomarkers for acute stroke management
- Fecal hemoglobin
- Sickle cell anemia
- Carbon nanotubes used for cancer diagnosis/treatment3
- Molecular tests for Influenza A/B and Strep
- Large-scale multiplexing
In addition, a growing number of smart devices and applications are being introduced to monitor health parameters (e.g., glucose, blood pressure, weight, pulse, electrocardiogram, physical activity, etc.). These emerging technological innovations in POCT offer a closer connection to the patient and are a big part of the transformation of the healthcare landscape.
POCT’s greatest asset, its rapid TAT, can speed diagnosis and treatment, allowing for faster clinical decisions across all areas of healthcare. The need for a rapid TAT has never been more apparent than in the COVID-19 pandemic. COVID-19 testing has showcased the perfect scenario where rapid TAT outweighs concern about testing sensitivity and specificity.
Small Tests Bring Big Challenges
Though there is certainty that POCT is on the rise and that it is valuable in certain scenarios, its oversight and management is quite complex because of the broad diversity of variables.
 |
Environment/LocationsIn a core lab, the testing environment is controlled and structured, whereas a POCT environment can vary widely and is not always controllable. The high variability can increase the risk of errors, which causes concern about test reliability. In addition, when testing takes place across multiple locations, perhaps different specialties, there are many diverse factors to take into account. |
 |
ConnectivityTo reap the benefit of a rapid TAT, POCT results must be automatically captured in the EMR/EHR for caregiver access. The connectivity required to integrate POCT results to affect a change in patient care can be challenging. |
 |
End User TrainingPOCT errors occur most often during the analytic phase of testing. This can be related to a lack of understanding or training of non-laboratory staff who are performing the testing. End users come from many different areas of healthcare and have various backgrounds and training, making oversight a challenge. In addition, there are CLIA-defined rules for training and monitoring competency thereafter that add to the complexity level, particularly when there are a large number of end users. |
Time to Embrace POCT
To paint a picture of many laboratories from “back in the day,” laboratorians were often located in the basement with no windows, had limited provider interaction, and had minimal patient contact. Also, historically speaking, laboratory professionals have avoided overall responsibility for POCT oversight because of its high level of complexity and the large number of remote factors that are difficult to control. Yet, laboratory professionals have also commiserated over their lack of recognition among healthcare peers and many have complained that the profession does not get the respect it deserves.
Today’s laboratories are embracing a paradigm shift—realizing that POCT is a powerful tool in the overall laboratory toolbox and that in the right places when speed is critical, POCT can have a positive impact on patient outcomes.

Knowledge Base Relevant for POCT
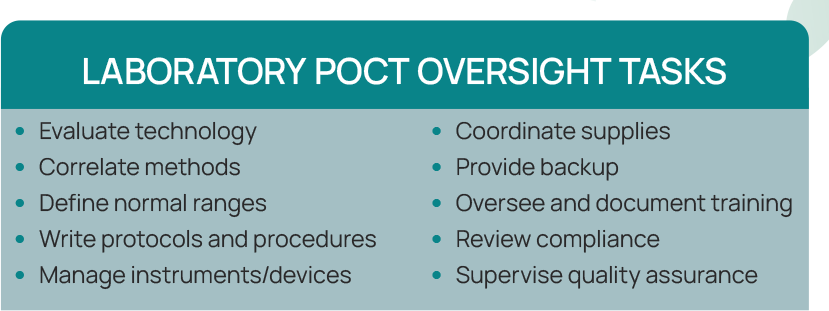
Laboratory professionals have the specific training and understanding needed to address POCT challenges and aid in decisions about best testing methodologies and placement of POCT where it makes sense for patients and providers (see Figure 3). POCT offers an opportunity for laboratory professionals to partner with providers to use POCT in the best patient scenarios.
The COVID-19 pandemic has brought attention to the medical laboratory scientist field as the healthcare heroes that are performing the testing. Yet, COVID-19 testing is riddled with complexities and misunderstandings. This fast-moving topic is an opportunity for laboratory professionals to share their laboratory knowledge and help providers and patients understand the caveats and complexities of testing and test interpretation.
 POCT will continue to grow, opening the door for laboratory professionals to use their knowledge to make sure POCT is performed just as accurately as any other lab test. Laboratory-trained professionals can help others understand the intricacies of accurate testing, including:
POCT will continue to grow, opening the door for laboratory professionals to use their knowledge to make sure POCT is performed just as accurately as any other lab test. Laboratory-trained professionals can help others understand the intricacies of accurate testing, including:
- Explaining testing discrepancies
- Recommending appropriate POCT devices
- Offering advice about which tests are appropriate to order
- Navigating POCT vendor relationships
 Laboratory professionals overseeing POCT have an opportunity to increase the profession’s visibility, and in their role of POCT oversight, function as:
Laboratory professionals overseeing POCT have an opportunity to increase the profession’s visibility, and in their role of POCT oversight, function as:
- Consultants
- Educators
- Key resources
- Part of the care team
The End User’s Perspective & Its Importance
To succeed as a leader in POCT management, it is beneficial to recognize the testing scenario from the end user’s perspective. Each individual has a unique point of view and opinions based on their life’s journey, education and training, and overall experiences. What is often not taken into account is that, although healthcare workers have taken different educational paths, the overall mission is to work together on the same team to take care of patients.
Siloed departments have been the norm for many years in healthcare—each area working independently with minimal interaction or understanding of each other’s roles. Laboratorians express frustration with phlebotomists and end users making seemingly obvious mistakes, such as not completely filling a Na+ citrate tube or wrapping one label sideways around three tubes, but is it not the lab’s responsibility to collaborate and teach proper technique? An approach of disdain or condescension does not promote a culture of teamwork.
Different Training Paths
As an end user example, the training path for a nurse is focused on the patient. The bulk of nursing studies and day-to-day activities are patient outcome oriented (see Figure 4). Goals are measured by patient time and patient achievements.

Conversely, the laboratory professional’s training is process-oriented, with a focus on details, precision, and following procedures. Laboratory goals are measured by accuracy and precision. This variation is for good reason. Nurses take care of patients and laboratory staff reports accurate results to guide diagnosis and treatments. But in today’s healthcare environment, it is abundantly clear that we need interdisciplinary teams working together that understand and respect each other’s perspectives in order to drive improved patient outcomes to support value-based care.
Role of Nursing in POCT as End Users
Laboratory testing is not seen as a traditional role for nursing. Not only does it take precious time away from the primary focus of patient care, but it also does not fit easily into a nursing workflow. Nurses are more familiar with the pre- and post-analytical steps of laboratory testing, such as specimen collection and acting based on results (i.e., initiating treatments), and less accustomed to analytical steps (e.g., quality control, proficiency testing, etc.). See Figure 5.

Role of Lab in Oversight of POCT
The laboratory professional’s role in management of a POCT program is as a knowledge resource. By setting a culture of mutual respect and encouraging open discussion and communication, a more effective POCT program is enabled (see Figure 6).
Start with Why
One of the best leadership tools is to create an understanding among clinical staff of why proper steps (e.g., QC, maintenance, etc.) are important, rather than taking the “you have to do QC or fail inspection” stance. Train end users about test limitations and potential interferences and the importance of evaluating results based on patient presentation.
Always include the why—why these steps are important to patient care.
Set Up POCT Activities with the End User in Mind
When you are implementing a POC test, it is important to consider the end user and how they will fit that POCT into their workflow. As a point-of-care coordinator (POCC), it is wise to streamline QA requirements to achieve goals using minimal resources that have maximum impact on patient quality. Consider the end user’s current workflow and discuss how POCT best fits. Workflow changes may be necessary to optimize POCT implementation, but strive for a minimal disruption of routine and determine the new workflow with end user input. QC, PT, and competency assessments take time away from patient care. Also, different locations, areas, and nursing units may have different workflows that can accommodate regulations in various ways and still be compliant.
Write policies and procedures in a user-friendly, easy-to-understand language, rather than in technical laboratory verbiage. If procedures are put in place that do not allow nursing units to implement POCT in ways that fit their workflow, this can lead to workarounds or noncompliance. Allow individual flexibility in implementation without being too stringent, keeping in mind the goal of error-prevention.
It is also wise to use technology wherever possible to prevent errors by including controls and QA monitors around weak steps that cannot be removed from the testing process (e.g., results cannot be approved without QC, operators not up-to-date on certification cannot approve results, etc.).
Encourage Continual Quality Improvement
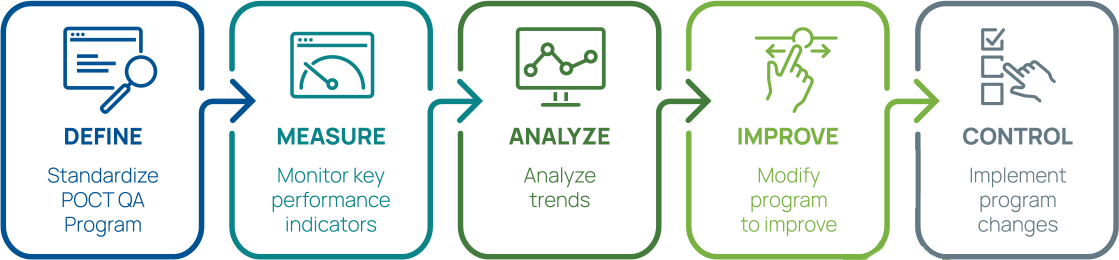
Create a culture that is not about pointing out errors, but about continually striving to improve. One tool available is the Lean Six Sigma 5 stages of DMAIC (pronounced “duh-may-ik”) for cyclic process improvement.4 See Figure 7. The planning stage involves forming an interdisciplinary POCT team, then cycles through defining, measuring, analyzing, improving, and controlling the processes. Analysis of key performance indicators will lead to development of new indicators to continue making improvements.
DMAIC: Improving Organization Performance
Encourage Self-management
Open and clear communication alongside readily available tools can promote self-management and further improve a POCT program. Having a POCT website or electronic folder on a shared drive can provide helpful tools for POCT end users. The site can be used to house policies and procedures, training and compliance forms, performance improvement goals and progress, committee minutes and agendas, and regulatory updates.4 Give the end users the tools they need to perform their role, and the laboratory can be available as a consultant.
Site self-inspections are recommended as part of a self-sufficient POCT end unit.4 Sites can utilize the same checklist that the POCC uses for a mock inspection to make sure their unit is not missing any important steps.
 More Strategies to Improve POCT Compliance
More Strategies to Improve POCT Compliance
Working together as a team to achieve rapid, accurate results that can improve patient care is a worthy goal. Some tactics that can support a teamwork effort include:
- Promoting self-management and recognition of the importance of each staff member’s role in patient care
- Implementing system changes to address compliance issues, rather than blaming the operator
- Regularly and clearly communicating policies, procedures, program goals, and expectations
- Creating a culture that accepts visibility in the end unit through laboratory visits and interaction4
POCT as an Opportunity to Demonstrate Value
The ongoing shift of policies and practices in the direction of value-based and patient-centered healthcare is bringing testing closer to the patient. These trends virtually ensure that the volume of testing performed outside of the core laboratory continues to grow. And as healthcare organizations change their models, the role of clinical laboratories—and how they serve their organizations—will also undergo change. Increasing sophistication and use of POCT is destined to play a major role in this new healthcare paradigm.
The need for experienced, knowledgeable oversight to achieve accurate POCT results so that its rapid TAT can be realized is an opportunity for laboratory professionals to gain visibility and to use their skills and training in a broader healthcare stance. Because of the inherent limitations and trade-off between speed and accuracy/precision, POCT must be diligently monitored so that the speedy results can positively impact patient care.
Laboratory expertise is vital to ensure testing is performed where it can have the most positive influence on patient outcomes and that quality results are achieved.
Laboratory professionals need to become involved and engaged in the management of POCT in order to showcase the laboratory’s contribution to the healthcare team and to improve the overall contribution of the laboratory. One way to achieve this is by effectively and collaboratively leading a POCT team. As the leader of a POCT team, it is important to develop a teamwork culture, take end users’ perspectives into account, and promote clear, open communication.
Orchard Point-of-Care Software Solution
Orchard Software offers Point-of-Care Testing (POCT) management and integration software that allows POC coordinators to manage their POCT program from a central location, addressing the challenges of remote POCT oversight. This means easy tracking of disparate devices across multiple locations, tracking operator competency assessments for hundreds to thousands of end users per device, interfacing and communicating with disparate POCT devices, and ensuring that care gaps are closed and POCT are automatically billed as the testing is completed. In addition, Orchard’s POCT solution is vendor-agnostic, includes decision support rules that improve laboratory productivity, and can help standardize POCT across locations. Orchard POC stands out from its competitors because its implementation is flexible enough to improve POCT workflows across many different types of healthcare organizations.
Orchard Point-of-Care Testing Network
Orchard Software is proud to announce its Point-of-Care Testing Network intended to help businesses integrate and connect point-of-care testing across multiple geographic locations, including rapid point-of-care testing for COVID-19. The Orchard Point-of-Care Testing Network can improve processes associated with point-of-care testing for any business that intends to track point-of-care test results, including skilled nursing and senior living facilities, nursing homes, educational institutions, airlines, etc.
The Orchard Point-of-Care Testing Network enables electronic test ordering and automated result reporting as well as automatic reflex ordering where indicated. In addition, the Point-of-Care Testing Network supports various government reporting requirements and provides integration to HHS, state health departments, and the Centers for Disease Control and Prevention (CDC). The solution enables facilities to manage point-ofcare testing devices from a central location, track point-of-care testing patient orders and results, meet CLIA requirements for point-of-care testing, and compile and report required data.
References
- Pennic, J. Top 10 Challenges, Issues and Opportunities Healthcare Executives Will Face in 2020. HIT Consultant. September 2019. Accessed at https://hitconsultant.net/2019/09/13/top-10-challenges-issuesand-opportunities-healthcare-executives-will-face-in-2020/#.X48-5NBKiUk
- Gami, U. Emerging Technologies for Point-of-Care (POCT) Testing: A future outlook for Scientists and Engineers. Conference: Symposium on Emerging Areas in Biosciences and Biomedical Technologies. January 2018
- Vashist, SK. Point-of-Care Diagnostics: Recent Advances and Trends. Biosensors (Basel). 2017;7(4):62. Published 2017 Dec 18. doi:10.3390/bios7040062
- Nichols, JH. The Nursing Lab Relationship in POCT: The Good, the Bad and the Ugly of Interdisciplinary Teams. April 4, 2019. Accessed at https://www.whitehatcom.com/POC_Group_Webinars_2019.htm

